Difficult PS segments
Nonanatomical resections in the PS segments - Diamond Technique
Mo Abu Hila
F.Cipriani
Parenchymal-sparing liver resections (PSLRs) have been advocated in the last years especially for colorectal liver metastases. (1-2) This approach allows radical resections with the maximum preservation of parenchyma decreasing the risk of postoperative liver failure, and favours future resections in case of recurrence extending survival in a now chronically managed disease. (3-5)
Both open PSLRs and laparoscopic PSLRs (LapPSLRs) for peripheral lesions are supported by encouraging results. However, their applicability for non-peripheral liver tumours is still debated. (6-8) Lesions requiring these resections are located elsewhere deep within the parenchyma, frequently in the posterosuperior segments, and therefore are difficult to approach in the absence of tactile feedback. (7,9)
The “diamond” technique" is intended to facilitate such resections with a laparoscopic approach without affecting the technical safety and the oncological efficiency of the procedure.
Patients are placed in the supine position. After positioning the right upper quadrant and epigastric ports, the inspection of liver surface is performed along with intraoperative ultrasonography.
Tumour size and location are evaluated to ensure favourable placement of the remaining ports. A 4/5-port configuration is fitted with a “L-shape” around the medial and inferior side of the tumour.
This port placement, along with the liver rotation favoured by a good mobilization, is intended to facilitate four transection planes running in line with the transection device. After insertion of all ports, ultrasonographic assessment of tumour relation to major vascular/biliary structures is performed.
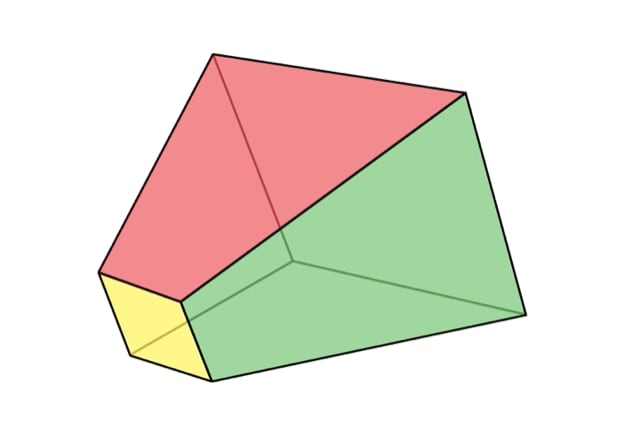
Key structures are marked with diathermy on the capsule. To achieve adequate resection margins, a “square-shaped” transection area is outlined at 2 cm nearly from the tumour, aiming for 10 mm tumour-free margin on each side of the lesion. The distance from the tumour can be slightly less in case of very small lesions, but at least 1 cm of distance is needed. Straight transection lines in a square shape are easier to follow, especially on deeper planes of dissection. The resection lines are identified as acoustic shadows on ultrasonography, allowing to evaluate the relation between the tumour and the intended resection lines throughout their length.
The transection is started with an energy shear dissector followed by an ultrasonic dissector when approaching the deeper planes. Two stitches positioned on the edges of the specimen (away from the tumour) may help in lifting and opening the resection line, thus reducing the disadvantages of a growing deep and narrow workspace.
To progressively bear toward the centre of the specimen is a well-known risk in open surgery. In laparoscopy this is further magnified by the absence of tactile feedback.
Although we conventionally call this the diamond technique due to the similarity of the final specimen with a diamond shape, we herein emphasize the need of continuous assessment and adjustment of the transection line aiming toward a semi-diamond “frustum shaped” specimen, rather than a complete diamond or a cone.
This is essential for achieving adequate tumour-free margin on both the lateral and basal transection planes. Repeated ultrasound and ultrasonic dissection both facilitate the development of millimetric readjustments of the dissection line. Whilst the lateral margins can be easily assessed, evaluation of the basal margin can be challenging. For this, ultrasonic measurement of the tumour location from the surface can estimate the depth of dissection needed, and the specimen can be scanned from the lateral side of the tumour. When the lower plane is reached, the tip of the laparoscopic grasper below the specimen can be detected on ultrasound permitting the evaluation of its relation with the inferior part of the tumour. In addition, careful ultrasonic dissection enables the identification of all structures deep in the parenchyma, which are then secured according to their size, thus ensuring haemostasis and biliostasis. Intermittent inflow control is performed during the dissection phase in the majority of cases. In case of small specimens, they are removed from a slightly enlarged port site instead of a Pfannenstiel incision, which is generally used for major resection or large specimens.
In 2015, the results achievable with the systematic adoption of this technique in a single centre have been analysed, and the outcomes disclosed by the authors reflect its safety, feasibility and oncologic efficacy (10). The study population comprised 49 LapPSLR (up to December 2014): the intra- and postoperative short-term outcomes were calculated for 24 isolated LapPSLR (not associated with any concurrent liver resection), whilst oncologic results were analysed for 24 LapPSLR performed for colorectal liver metastases. Lesions were located in segments 8, 7, 4a, and 3 in 51%, 8.2%, 36.7%, and 4.1% of cases, respectively.
The authors report a relatively low rate of conversion to open, that was necessary in 8% of the procedures (4 patients). These results are similar, and not increased, to the conversion rates reported for both minor laparoscopic liver resections for favorably located lesions and laparoscopic major hepatectomies. (11-13) Unfavourable intraoperative accidents (according to the Satava approach to Surgical Error Evaluation adapted for laparoscopic liver resections) occurred in 20.8% (5 patients), however, without major accidents with relevant clinical effect or consequences: 3 grade 1 events (2 small bowel serosal tear oversawn, and 1 gallbladder perforation requiring cholecystectomy), 1 grade 2 event (major hepatic vein bleeding requiring conversion); no grade 3 events (14). Median operative time and blood loss were 215 minutes and 225 mL, respectively. Pringle maneuver was used in 75% of cases. Post-operative 90-day mortality was nil and morbidity rate was 12.5%: 1 wound hematoma (mild); 1 transient atrial fibrillation (moderate), and 1 bile leak managed with ERCP and endobiliary stent insertion (severe). Bleeding and bile leak are commonly feared complications in liver surgery, especially in central resections (15). These concerns are even more significant when adopting the laparoscopic approach. (16) In their series, however, only 1 patient was converted because of bleeding and 1 postoperative bile leak has been observed. The median postoperative stay was 3 days.
Regarding the oncologic results, the median tumor-free margin was 4 mm and 100% R0 rate was achieved for all LapPSLRs with curative intent. This result compares favourably with the outcomes reported by Kazaryan and colleagues in their series (3 mm; range 0 to 13 mm) (17). Together with the 3-year overall, recurrence-free, and disease-free survival rates achieved (100%, 65.2%, and 69.6%, respectively), the results are also similar to the average outcomes reported for laparoscopic and open liver resections for CRLM. (18-20)
These outcomes support the adoption of the “diamond” technique to accomplish safe and oncologically radical parenchymal-sparing resections for nonperipheral liver lesions through a laparoscopic approach. Currently, PSLRs for nonperipheral tumors are still retained for open surgery in the majority of hepatobiliary centers, although the laparoscopic approach for liver re- sections has undergone a huge spread. The lack of experience can lead to a preference for the traditional open approach, or to the hazard of widening the extension of the hepatectomy and major laparoscopic liver resections unjustifiably being carried out for these cases. However, this study showed that the outcomes of LapPSLRs for nonperipheral lesions can resemble open PSLR. As such, the disclosure of these favorable results should encourage hepatobiliary surgeons to develop their skills in the laparoscopic management of these lesions, and this technique might help tackle those lesions with fewer difficulties.