Difficult PS segments: general aspects
Mathieu D'Hondt
To date, most laparoscopic liver resections have been directed to easily accessible lesions in the anterolateral segments of the liver (Segments II, III, IVB, V, VI). These type of resections have been considered suitable for a laparoscopic approach.(1-3)
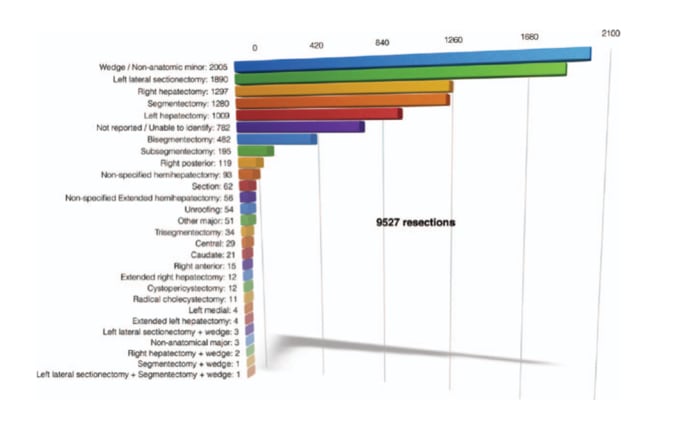
A recent world review indicated that the number of cases of laparoscopic resections is increasing exponentionally, however most of the reported cases involved minor resections, including wedge resections and left lateral sectionectomies (4).
Diffusion of laparoscopic liver resection (LLR) has been hindered by several technical difficulties. According to the Louisville Statement, laparoscopic major hepatectomy is a heterogeneous category that includes traditional trisectionectomies, hemi-hepatectomies and the technically challenging resection of segments 4a, 7, and 8.(4) However, the Southampton group has shown different short-term outcomes when comparing laparoscopic ‘‘traditional’’ major hepatectomy (LTMH) and laparoscopic ‘‘posterosuperior’’ major hepatectomy (LPMH).(5)
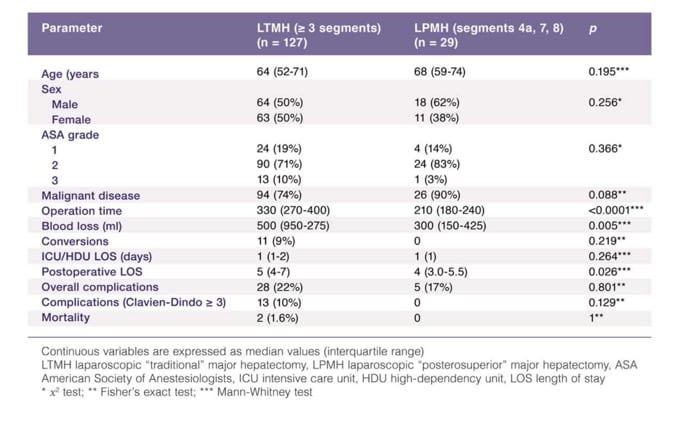
It seems approapriate to create two subcategories of laparoscopic major hepatectomy. Athough major hepatectomies have traditionally been defined as those including three or more continuous Couinaud’s segments with those involving two or less classified as minor, LLRs in the posterosuperior segments are considered technically major resections to differentiate them from minor resections and acknowledge their difficulty.
However, there are major concerns regarding hemostasis at the transection plane, controlling hemorrhage, and the limited working space and visualization laparoscopic LLRs in the posterosuperior segments of the liver (Segments 4A, S8, S7, upper part S6), (6-7). The complexity of LLRs in the posterosuperior segments is also reflected in the difficulty score for laparoscopic liver resections.(8) The difficulty of a LLR is calculated by adding an applicable score for the extent of liver resection, tumor location, liver function, tumor size and tumor proximity to major vessels. Tumors located in S8 or S7 earn the highest score, due to the difficulties presented by its location.
Recently, several centers with advanced experience in laparoscopic liver surgery have published on laparoscopic liver resections in these difficult segments (5, 9-16). Still, several reports indicate that patients with tumors of the posterosuperior segments are more likely to undergo hemihepatectomy instead of a nonanatomical resection or anatomical segmentectomy.(17,18)
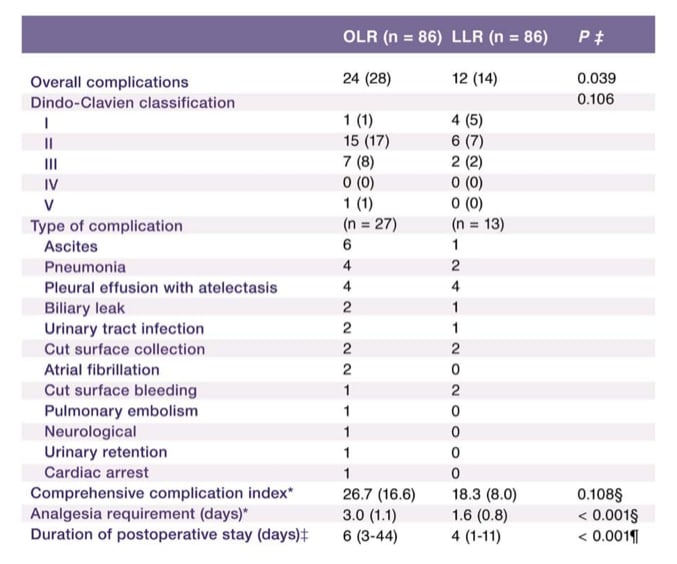
In 2017 a large multicenter comparative analysis was published comparing laparoscopic and open liver resections in the posterosuperior segments. (19) A Propensity score-matched analysis was used to match groups for known confounders. Perioperative outcomes including complications were assessed and survival was analysed. After propensity score-matched analysis, 86 patients remained in both groups. Overall postoperative complication rates were significantly higher after open liver resection compared with LLR and mean duration of required analgesia and the median duration of postoperative hospital stay were significantly shorter in the LLR group. The 3-year recurrence-free survival rates for patients with hepatocellular carcinoma (37 per cent for open resection versus 30 per cent for LLR; P =0⋅534) and those with colorectal liver metastases (36 versus 36 per cent respectively; P =0⋅440) were not significantly different between the groups. The authors concluded that LLRs in the posterosuperior segments are feasible and are associated with less complications without compromising oncologic outcomes.
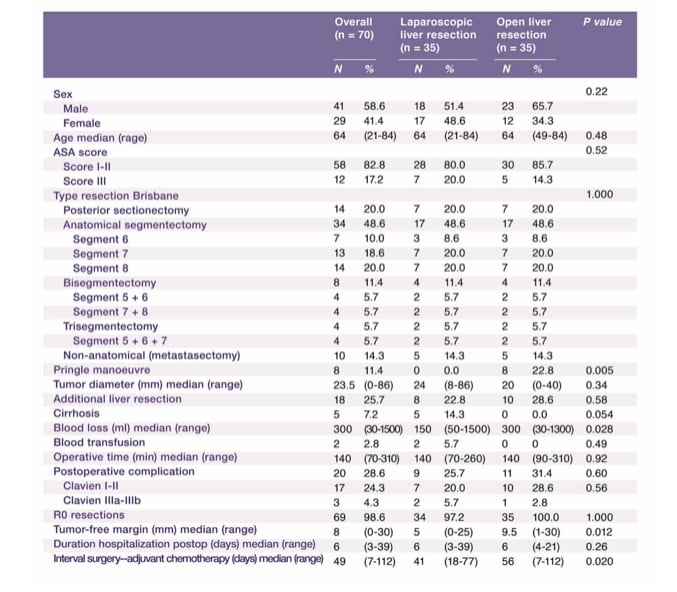
We recently published a comparative study comparing LLRs in the posterosuperior segments with identical open liver resections in the posterosuperior segments. (15) Laparoscopic cases were case-matched with those who had an identical open procedure during the same period based on tumor location (same segment) and the Brisbane classification of the resection.
Both groups were comparable for age, sex, ASA score, maximum tumor diameter, and number of patients with additional liver resections outside the posterior segments. Operative time was similar in both groups (median 140 min; p = 0.92). Blood loss was less in the LLR-group (median: 150 vs. 300 ml in OLR-group). Median hospital stay was 6 days in both groups. There was no significant difference in postoperative complications (OLR-group:
31.4% vs. LLR-group: 25.7%; p = 0.60). Patients undergoing LLR were treated with chemotherapy sooner compared to those undergoing open resection (41 vs. 56 days,
p = 0.02). Our study suggests that laparoscopic parenchymal preserving liver resections in the PS segments can be performed with comparable short-term outcomes as similar open resections. The shorter interval to chemotherapy might provide long-term oncologic benefits in patients who underwent LLR.
On November 1st 2017, the ORANGE SEGMENTS - Trial opened (NCT03270917). This international and multicentre trial is a prospective, double blinded, randomized controlled study comparing patients undergoing parenchymal preserving resection of postero-superior liver segments (involving one or two of segments 4a, 7, 8). All patients will be participating in an enhanced recovery programme. Primary outcome of the study is time to functional recovery. Secondary study parameters include hospital length of stay, intraoperative blood loss, operation time, liver specific morbidity, readmission percentage, resection margin, quality of life, body image and cosmesis , reasons for delay of discharge after functional recovery, long term incidence of incisional hernias, hospital and societal costs during one year, time to adjuvant chemotherapy initiation, overall five-year survival. Based on a difference of 2 days in time to functional recovery between the groups, with 80% power, the study will require 125 patients in each arm of the trial. Hence the international total recruitment will be 250 patients.(20).